Hi there
This is my first post on this forum.
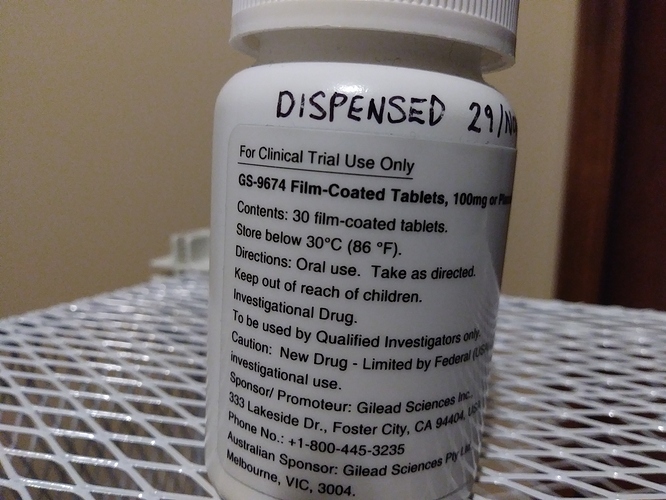
I too am on the GS-9674 Phase 3 trial based in Vancouver BC CANADA (I live in Victoria though). I started last year in February 2020, and have passed the one year mark.
I was convinced that I was on the placebo, but the research coordinator thought otherwise as my LFT numbers were normalized to a degree… at least for the first few months. They started progressively going up since about last August. Overall, my number were substantially reduced after being put on 750mg ursodial, about 1/2 year after initial diagnosis. I was diagnosed in March/April 2017 when I was 47. I am female and don’t have IBD and am vegan. This latter bit definitely helped my situation especially my colonscopies. I became plant based for ethical reasons but the health benefits are definitely prominent (plant based limiting processed foods).
Anyway, the past couple of weeks I started feeling worse (nature of the disease as you all know) – this time it was more than RUQ pain, but was accompanied by slight nausea. At the end of two weeks, I felt it time to use my blood req to check my levels. As suspected, things were a little out of whack.
First time with my ALP numbers being this high…not tragic, but in the mid-400s and my eosophils are high and RDW low. I don’t want to take antibiotics unnecessarily so my gastro/hep and I agreed that I would gauge through tests along with fever/chills.
The pruritis increased but was unbearable last night and my skin is raw. It is so frustrating as it happened on the weekend and my gastro isn’t around, and neither is the research coordinator. I went through an NP and the gastro on call won’t give me anything because he doesn’t want me to be kicked out of the trial but I know that bile acid sequestrants won’t do that - I was even offered this by the research gastro/hep and research coordinator. So frustrating because I couldn’t speak and answer the GOC questions directly. Now I have to have 2 more sleepless days and nights with less skin until I can speak with my specialist.
Anyone else been offered a sequestrant to deal with the pruritis from the trial? I know mine isn’t drug-related but rather just the course of the disease.
Fortunately until now, the pruritis was over less than an hour each time and localized. Now it is all over.
I know most mention bottom of feet and hands but I itch in the groin, scalp, mid-section, back, buttocks, legs and arms… basically everywhere including my neck. Anyone else have it all over?
I do get temporary relief from a lukewarm bath but it doesn’t last long.
Thanks for listening and hopefully for responding to some of my questions!