Hi all. I haven’t been on here in a while. Was just getting on with the business of living. Have a question. My latest MRI/ Mrcp shows cirrhosis is the same but a small blockage is starting in one of my large bile ducts. I have large duct PSC. Is there anything I can do to reverse it or stop it from getting bigger? I started taking Krill Oil and Coenzyme Q10 as I also have arthritis…that won’t make it worse will it?
Hi Buttercup,
Sorry you are showing a blockage. Unfortunately there’s nothing you can do to reverse or stop it from getting bigger. If your bilirubin numbers start to significantly climb and/or you start having some pretty serious itching, an ERCP may be in order. They can then go in during that procedure and dilate the duct and clean it out so the bile will flow again. As the disease progresses though you may start having the smaller ducts up in the liver itself that will get blocked and there’s not much they can do then. I’m not sure about Krill Oil’s effect on PSC.
Take care.
Mark, Moderator
PSC 2011 / Liver Transplant 7-2015
Thanks. What is an ERCP?
Buttercup,
I’m pasting in some information on ERCP from several web sites as well as some links you may want to check out…You will probably become very familiar with this procedure as the disease progresses. It’s very important you find a physician preferably at a transplant hospital that does this all the time as it’s a very delicate and invasive procedure. Don’t just get any ole GI doctor to do this.
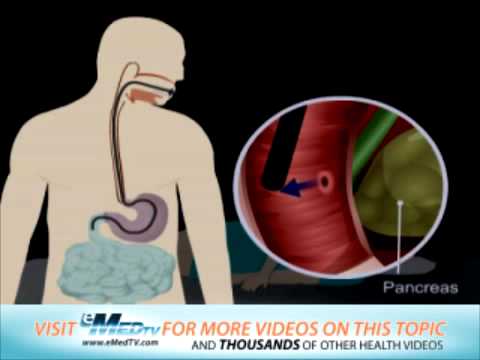
What is ERCP (Endoscopic Retrograde Cholangio-Pancreatography)?ERCP
is a procedure that enables your physician to examine the pancreatic
and bile ducts. A bendable, lighted tube (endoscope) about the thickness
of your index finger is placed through your mouth and into your stomach
and first part of the small intestine (duodenum). In the duodenum a
small opening is identified (ampulla) and a small plastic tube (cannula)
is passed through the endoscope and into this opening. Dye (contrast
material) is injected and X-rays are taken to study the ducts of the
pancreas and liver.Why is an ERCP Performed?ERCP is most
commonly performed to diagnose conditions of the pancreas or bile
ducts, and is also used to treat those conditions. It is used to
evaluate symptoms suggestive of disease in these organs, or to further
clarify abnormal results from blood tests or imaging tests such as
ultrasound or CT scan. The most common reasons to do ERCP include
abdominal pain, weight loss, jaundice (yellowing of the skin), or an
ultrasound or CT scan that shows stones or a mass in these organs.ERCP
may be used before or after gallbladder surgery to assist in the
performance of that operation. Bile duct stones can be diagnosed and
removed with an ERCP. Tumors, both cancerous and noncancerous, can be
diagnosed and then treated with indwelling plastic tubes that are used
to bypass a blockage of the bile duct. Complications from gallbladder
surgery can also sometimes be diagnosed and treated with ERCP.In
patients with suspected or known pancreatic disease, ERCP will help
determine the need for surgery or the best type of surgical procedure to
be performed. Occasionally, pancreatic stones can be removed by ERCP.What Preparation is Required?Your
stomach must be empty, so you should not eat or drink anything for
approximately 8 hours before the examination. Your physician will be
more specific about the time to begin fasting depending on the time of
day that your test is scheduled.Your current medications may need
to be adjusted or avoided. Most medications can be continued as usual.
Medication use such as aspirin, Vitamin E, non-steroidal
anti-inflammatories, blood thinners and insulin should be discussed with
your physician prior to the examination as well as any other medication
you might be taking. It is therefore best to inform your physician of
any allergies to medications, iodine, or shellfish. It is essential that
you alert your physician if you require antibiotics prior to undergoing
dental procedures, since you may also require antibiotics prior to
ERCP.Also, if you have any major diseases, such as heart or lung
disease that may require special attention during the procedure, discuss
this with your physician.To make the examination comfortable,
you will be sedated during the procedure, and, therefore, you will need
someone to drive you home afterward. Sedatives will affect your judgment
and reflexes for the rest of the day, so you should not drive or
operate machinery until the next day.
Here are some helpful links that will give you a better understanding of the procedure.
Mark
PSC 2011 / Liver Transplant 7-2015
Buttercup,
Mark gave some good advice. I think the only way it can be opened is with the ERCP. Once in, the doc can decide whether a stent is needed or if the blockage can be opened with a balloon.
Both have disadvantages-a stent needs to come out in several months. A balloon dilation may not have the staying power of a stent. I had a balloon dilation in March 2015 and have been good since.
Keep in mind that an ERCP is not without risk. It can cause pancreatitis.
But the advantages of an ERCP outweigh this risk.
Jeff
Thanks so much Mark! This really explain ERCP! The blockage I have apparently is just starting so hopefully it will be a while before I need one. Wish there was something I could do to stop it from blocking up anymore and to reverse it but maybe the Scientists will find a way. Thanks again.
Thanks Jeff for replying to my enquiry! Appreciate the input. 
Personally I get an ERCP with balloon dialation every 6 weeks with an overnight hospital stay for observation, as I have many blockages including the common bile duct. Typically, you will be given an antibiotic such as ciprofloxacin for around 5 days post op to avoid infection. Also, because this is a strong antibiotic, it may cause you to get a yeast infection, so you may also get fluconizole to prevent/treat that. Here are some things to look out for:
- jaundice (skin and eyes turn yellow)
- if you get very itchy
- if your poops turn white/clay colored (gross I know, but this indicates a blockage as bile gives your #2 it’s color)
- greasy/floating poops (again gross, sorry. But this also indicates you have a problem as fat is not water soluble, so bile salts break it down to be water soluble and if there is a blockage the bile can’t get out to do it’s job.
Also, while ERCP is the only way to treat the blockage, there is a medication called actigall/ursodiol which thins bile to make it easier for it to flow through narrowed ducts.
Feel free to contact me if you have any questions! 
Thanks schmoop! Appreciate the information 
Hi Schmoop - with the every 6 wk ERCPs, are you becoming resistant to the sedation? For several years, I was having stent changes every 3 mths (till this past spring - we’re trying for 5-6 mths now). Last summer/fall had a few ERCPs within a 4 mth period when I was quite ill. I’m becoming more and more wakeful with each ERCP - not very pleasant! I’ve had 23 so far, used to be a walk in the park - but now I’m anxious about it. When given additional sedation to keep me under, I’m extremely nauseous for hours afterward. Coming up again early Sept.
One suggestion. Ask the doctor to order a “Scopes Patch” put just behind the ear for nausea just before they take you back for the procedure. Also my doc used general anesthesia instead of the MAC type. I never knew anything until I woke up. Much better for me.
Mark
Thanks Mark. One of my specialists suggested that, but surgeon said GA won’t happen for a scoping procedure. They did however try me last time on Ketamine and propofol. Horrible. Never again - was like a ‘bad trip’. Turns out I was still waking up. The procedure had taken longer than usual and I was horribly nauseous afterward from the amount of medication needed. I’ll ask about the patch though.
Sorry Alix that the surgeon would not allow the GA. Your insurance should surely pay for it. It sounds to me he’s being a bit stubborn. Surely your specialist could intervene in your behalf and request that further scopes be done under GA. You are the patient, if it were me I would demand it unless he could give a sound medical reason why not. If the anesthesiologist doctor approves it well then he needs to keep his opinion to himself. Of course, I’m no doctor and he may have his good reasons, but I for one don’t want to be waking up during a procedure like an ERCP. Interestingly if you eventually get a transplant you will not have to worry about ERCP’s anymore, at least for liver problems. They reroute your plumbing and have your bile ducts feeding directly into the colon. You get a plumbing makeover. 
Mark
PSC 2011 / Liver Transplant 7-2015
I believe it’s hospital policy that doesn’t allow use of the ORs for scoping and the surgeon said GA cannot be administered in the ERCP room. The surgeon who did my last ERCP (in his absence) also told me same. I’ll see how the next ERCP goes, I haven’t had the usual sedation since last Nov, hopefully I’ll have less resistance to it. If it doesn’t go well, I will insist on an anaesthesiology consult, that’s for certain.
Interesting about the rerouting of bile ducts. Do bile ducts not feed into duodenum, or is it colon?
Alix,
I did a little research and the technique you mentioned is done sometimes into the duodenum, but at least from this article with PSC patients the Roux-en-Y hepaticojejunostomy technique is the preferred method. See below for part of an article I found I’m inserting. Here’s the link for the full article though. Article
Roux-en-Y hepaticojejunostomy (RYHJ): In this technique, a loop of small bowel 10-20 cm distal to the ligament of Treitz is divided and brought up to the donor bile duct. An end to side anastomosis is then completed between the two (Image 2). The RYHJ is a preferred technique when the donor bile duct diameter is small (pediatric, split liver and living donor transplants) and in patients with extrahepatic biliary disease (eg. primary sclerosing cholangitis, Caroli’s disease and cholangio-carcinoma).
There are unique complications associated with type of biliary reconstruction that are related to the surgical enteric anastomosis. This approach adds to the operative time because it involves small bowel resection and anastomosis. In addition, there is an increase the risk of peritonitis due to enteric leaks and bleeding complications. These complications are exacerbated by the high venous pressure associated with portal hypertension in some patients. There is also an increase the risk of developing ascending cholangitis from contamination with gut flora. Further, subsequent endoscopic intervention to treat bile duct narrowing is difficult if not impossible.
Hope this helps.
Mark
Thanks Mark, very informative!
Hey yall!
We have had lots of blockages (and up until finding our relief…lots of ercp’s)
We took a step of faith and had another baby. Through that and nursing again I researched that breast duct tissue is like bile duct tissue and with blockages in the breast ducts you can use sunflower or soy lecithin to clear them and open them back up-keep them flexible and slippery.
We have successfully used sunflower lecithin to clear hubbys’ blockages and keep him for a year without needing ercp’s. His liver enzyme levels have reduced and some are in NORMAL RANGE!!! He takes the sunflower lecithin twice a day. I can ask him what his dosage is right now.
over a year ago they told us we were looking at transplant within a year to three years. We were shocked a month ago when the doctor said some levels were normal again…they have not been that in over 4 years.
All I can say Mommymoses is WOW!..What a discovery you have made. This certainly sounds like something that folks may want to try. Applying the same principle to clear breast milk ducts to the livers bile ducts is something. I hope our folks will give us some feedback on this and see if it works for others as it appears to have worked for your dear husband. Keep up the good work.
Mark
PSC 2011 / Liver Transplant 7-2015
Nice, mommymoses. So glad your hubby is better. I like hearing success stories.
Jeff
Sorry for the late reply, but I don’t think I’m resistant to the sedation. I do get extremely nauseous and normally vomit bile when I wake up. But now I get them every 8-10 weeks so it’s getting a little better.